Pancreatic Cancer: What You Need to Know
Understanding Pancreatic Cancer
Pancreatic cancer makes up about 3 percent of all cancers but causes around 7 percent of cancer deaths in the U.S. It is the third leading cause of cancer-related death and is often diagnosed late due to vague symptoms and its hidden location deep in the abdomen.
More than half of cases are found after the cancer has spread, limiting treatment options. Unlike cancers with routine screening, pancreatic cancer grows silently. Its resistance to standard treatments and rapid progression make early recognition and informed action critical
What Is Pancreatic Cancer?
Pancreatic cancer begins in the tissues of the pancreas, a small organ hidden deep behind the stomach. It plays two vital roles: making enzymes that help digest food and producing hormones like insulin that regulate blood sugar.
Cancer in this area often spreads before symptoms appear. That is why most people are diagnosed late.
This type of cancer grows in silence. It is rarely found during routine checkups, and imaging tests do not always catch it early.
Doctors classify it by where it starts. Most tumors begin in the exocrine cells, which help with digestion. A smaller number start in the endocrine cells, which control hormones.
Each type grows differently and responds differently to treatment. Knowing the exact type matters for planning care and making informed decisions.
How the Pancreas Functions in the Body
The pancreas is often overlooked, yet it works quietly every day to keep the body balanced. It releases enzymes into the small intestine to break down fats, proteins, and carbs. It also produces hormones like insulin and glucagon, which control blood sugar levels.
As people age, the pancreas may slow down. Inflammation, scar tissue, or unnoticed damage from years of wear can make it more vulnerable to disease. These small changes can set the stage for cancer, even in people with no family history.
Understanding how the pancreas functions helps explain why pancreatic cancer is hard to detect early. The signs are often confused with common problems like indigestion, aging, or blood sugar shifts.
How Pancreatic Cancer Develops
Pancreatic cancer usually begins with small mutations in the cells lining the ducts of the pancreas. These cells may grow abnormally for years before forming a tumor. Early changes often go unnoticed, especially in older adults whose bodies already show signs of age-related decline.
Unlike skin or colon cancer, pancreatic cancer does not have a clear path to early detection. There are no standard screening tests. By the time symptoms appear, the cancer has often spread to nearby organs, nerves, or blood vessels.
Chronic inflammation, such as from long-term pancreatitis, can create an environment where cancer is more likely to form. So can past exposure to certain chemicals, smoking, or even long-term type 2 diabetes.
In some cases, precancerous cysts slowly evolve into cancer over many years. These can be seen on scans but are often dismissed as harmless until it’s too late.
Can Pancreatic Cancer Be Cured?
Most pancreatic cancers are not curable once they are advanced. Only a small number of people are diagnosed early enough for surgery to remove the tumor completely. Even then, the risk of recurrence remains high.
Cure is tied to timing. If the cancer is found before it spreads, there is a chance for long-term survival. But because the pancreas sits deep in the abdomen and early signs are vague, most cases are found too late for curative treatment.
Older adults often have other health conditions that make aggressive treatment harder to tolerate. For them, “cure” may not be the goal. Instead, quality of life, comfort, and having control over end-of-life decisions become just as important.

Is Pancreatic Cancer Hereditary?
Most pancreatic cancers happen by chance, but about 10 to 15 percent are linked to inherited genetic changes. These mutations often run silently through families, sometimes masked by vague causes of death like “organ failure” or “stomach issues” in older relatives.
Mutations in BRCA1, BRCA2, and other genes like PALB2 or CDKN2A can raise the risk. These are the same genes linked to breast and ovarian cancers. People with a strong family history of any of these may carry hidden risk, even if no one in the family ever had pancreatic cancer.
Older adults are rarely offered genetic testing, especially after a diagnosis. But knowing if a cancer is hereditary can help inform children, grandchildren, and even guide future screening or donation decisions.
What Is the Best Treatment for Pancreatic Cancer?
The best treatment for pancreatic cancer depends on the stage at diagnosis, overall health, and personal goals. For early-stage cancer, surgery followed by chemotherapy may offer a chance at longer survival. But only a small percentage of patients qualify for this option.
Many older adults face a harder decision. Surgery can be complex and recovery is often long. Chemotherapy may offer more time, but with side effects that impact daily life. Some people decide that comfort is more important than aggressive treatment.
There is no one-size-fits-all answer. What matters most is aligning treatment with the patient’s values, priorities, and the reality of their remaining time.
Surgery, Radiation, and Chemotherapy
Surgery is the only potential cure for pancreatic cancer, but fewer than 20 percent of patients qualify due to late-stage diagnosis (Hirshberg Foundation). The Whipple procedure is most common but involves major recovery, especially for older adults.
Radiation is mainly used for symptom relief or to shrink tumors before surgery. Chemotherapy, including FOLFIRINOX or gemcitabine, is common but often causes fatigue, nausea, and low immunity (Mayo Clinic). For some, these side effects outweigh the benefits.
Targeted Therapies and Immunotherapy
Targeted therapies and immunotherapy help only a small group of pancreatic cancer patients with specific genetic mutations. According to the NIH, less than 10 percent of patients have tumors with markers like MSI-H or BRCA mutations that respond to these treatments. Most pancreatic tumors resist immunotherapy due to their dense structure and low immune activity.
What Are the Early Symptoms of Pancreatic Cancer?
Early signs of pancreatic cancer are often subtle and easily missed. Back pain, especially dull pain in the mid or lower back, can occur when tumors press on nearby nerves. New-onset type 2 diabetes in adults over 60 without weight gain may also signal pancreatic cancer.
Other early symptoms include unexplained weight loss, fatigue, changes in stool (greasy or pale), jaundice, and appetite loss. These symptoms are often mistaken for aging or digestive issues, leading to delayed diagnosis. When several symptoms appear together, especially in older adults, they warrant medical attention.
Older adults may think these are just signs of getting older. But when several symptoms show up together, it is worth asking questions. The quiet nature of early pancreatic cancer means it is often the family not the patient who first sees something is wrong.
Digestive and Symptoms
Digestive symptoms are among the earliest clues, but they are often mistaken for routine discomfort. Bloating after meals, indigestion that does not improve, or a sudden feeling of fullness after eating just a small amount can all point to a growing tumor pressing on nearby organs.
Changes in bowel habits are also common. Stools may become greasy, float, or smell unusually foul due to poor fat absorption. These signs are linked to blocked pancreatic enzymes, but most people do not realize their stool is telling them something serious.
Symptoms such as unexplained fatigue, night sweats, or low-grade fevers are often brushed off. These can signal that the immune system is responding to cancer, even before it is detectable on scans.
In older adults, symptoms may blend into other health issues or be misattributed to medication side effects. Slower digestion, sleep disruption, or shifts in blood sugar may seem unrelated. These subtle red flags are often missed in routine checkups.
Families and caregivers are often the ones who notice patterns, and their observations can make all the difference.
Survival Rates and Prognosis: Are Outcomes Improving?
Pancreatic cancer has one of the lowest survival rates of all major cancers. The overall five-year survival rate is less than 13 percent. When diagnosed at an advanced stage—which occurs in over half of all cases—median survival is often measured in months.
Progress is being made through better imaging, surgical techniques, and molecular research. However, access to these advances is uneven. Patients treated at high-volume cancer centers typically experience better outcomes than those treated in under-resourced or rural facilities.
Older patients are less likely to be included in clinical trials. Their outcomes are often underreported, which skews the data and limits progress in care planning for aging populations. This underrepresentation is documented in the Journal of Geriatric Oncology, which notes a critical gap in research for older adults facing cancer diagnoses (NIH).
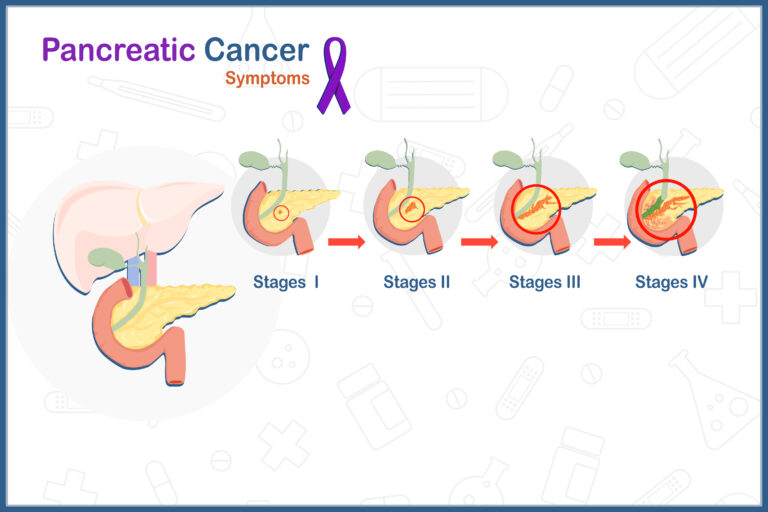
Survival Statistics by Stage and Type
Survival rates for pancreatic cancer vary greatly depending on how far the disease has spread at the time of diagnosis. Localized tumors, which are confined to the pancreas, have the highest survival rates. According to the American Cancer Society, about 44 percent of patients with localized pancreatic cancer survive at least one year, and roughly 20 percent survive five years or more.
When the cancer has spread to nearby tissues or lymph nodes (regional stage), one-year survival drops significantly, and long-term survival becomes rare. For distant-stage cancer, where it has spread to organs like the liver or lungs, median survival is often less than six months.
Tumor type also plays a role. The most common form, pancreatic ductal adenocarcinoma, is aggressive and fast-growing. In contrast, pancreatic neuroendocrine tumors tend to grow more slowly and may respond better to certain treatments, offering some patients a longer prognosis.
Understanding the stage and tumor type is essential for setting expectations and guiding decisions about treatment and care.
Geographic and Anatomical Patterns of Pancreatic Cancer
Pancreatic cancer incidence varies geographically, with higher rates observed in more developed regions. In the United States, the age-adjusted incidence rate is approximately 13.8 per 100,000 individuals per year, based on data from 2018 to 2022 (SEER – National Cancer Institute).
Globally, the highest incidence rates are found in Europe (7.7 per 100,000) and North America (7.6 per 100,000), while the lowest rates are observed in Africa (2.2 per 100,000) (NCBI – Global Pancreatic Cancer Burden).
Anatomically, about 65% of pancreatic cancers occur in the head of the pancreas, around 15% in the body and tail, and the remaining cases involve the entire organ (NCBI – Patterns of Pancreatic Cancer). Tumors in the head often cause earlier symptoms such as jaundice, leading to earlier detection. Tumors in the body or tail are typically found later, as they often grow without noticeable signs.
These geographic and anatomical patterns underscore the need for earlier detection efforts, particularly in underserved areas and in individuals at higher risk.
Questions to Ask Your Oncologist
It’s important to ask your doctor directly about what lies ahead, how treatment will affect your life, and what options are truly available. These questions are designed to help you get clear, honest information that reflects your health, your age, and your goals.
- What type and stage of pancreatic cancer do I have, and what does that mean for my treatment options?
- What experience do you have treating patients with this specific type and stage of pancreatic cancer?
- What are the benefits and risks of each treatment option based on my age and health?
- Am I a candidate for surgery, and if not, why?
- Should I consider a clinical trial, and how do I find one that fits my case?
- Should my tumor be tested for genetic mutations or biomarkers to guide treatment? (Learn more about biomarkers Here)
- What can I expect in the next few months, physically and emotionally?
- How will treatment affect my ability to live at home or care for myself?
- What kind of palliative support is available now to manage symptoms and side effects?
- How will we know if treatment is working, and when will we reassess?
Knowledge Is Power
Pancreatic cancer often arrives without warning and leaves little time to plan. But information, even when the news is difficult, offers something valuable—clarity. Knowing the stage, the options, and what to expect allows patients and families to make choices based on truth, not fear.
For some, that means pursuing every treatment available. For others, it means focusing on comfort, family, and time. There is no right answer—only the answer that aligns with your values.
What matters most is making choices that reflect how you want to live, be remembered, and supported through each stage of the journey.

