Breaking the Code: Unmasking Your Health Secrets with Biomarker Testing
The Undeniable Progress of Biomarker Testing
The American Cancer Society Cancer Action Network (ACS CAN) recently did a web-based survey of over 1200 cancer patients to help better see the impact of biomarker testing. In their survey, they found that:
- 49% of those surveyed have already had biomarker testing for their cancer which is a significant increase from 39% during the 2020 survey.
- 77% of those who have had biomarker testing agreed that it gave valuable information that improved their providers’ ability to treat the patient’s cancer.
- 53% say they are more likely to recover because of the biomarker testing.
- 50% say they were able to avoid unnecessary treatments or procedures because they completed biomarker testing.
- Biomarker testing was covered by insurance for 76% of those who had the test and 50% had no out-of-pocket costs.
- 84% of those who had biomarker testing say their provider initiated the process.
- The result of biomarker testing led to changes in treatment for 23% of those surveyed and 3% were able to enroll in the clinical trial.
Understanding Biomarkers and Testing
- Companion diagnostic test
- Genomic testing or profiling
- Genome sequencing
- Molecular testing or profiling
- Next generation sequencing
- Somatic testing
- Tumor testing
- Tumor genetic or marker testing
- Tumor subtyping
But at the end of the day, they are all the same things. A precision approach that is utilized for measuring the risk of recurrence, monitoring the response to treatment, detecting cancer, and aiding in treatment selection. When utilizing biomarker testing, there are stand-out benefits such as:
- Improved patient outcomes and optimal treatment for every individual
- Socioeconomic benefits include shorter hospital stays and overall better quality of life.
- Cost efficiency due to more targeted therapies that reduce time and resources spent on ineffective treatments.
- Early cancer detection, survival rates increase significantly when found early.
Biomarker testing examples can include blood pressure tests, x-ray results, CAT scan results, pulse, liquid biopsy (blood test for cancer detection), or the testing of tumor molecules. If a patient gets a tissue sample taken, it will be taken during surgery or biopsy. Certain biomarker testing can even help medical professionals diagnose and monitor cancer before and after any treatment to help maintain patient health.
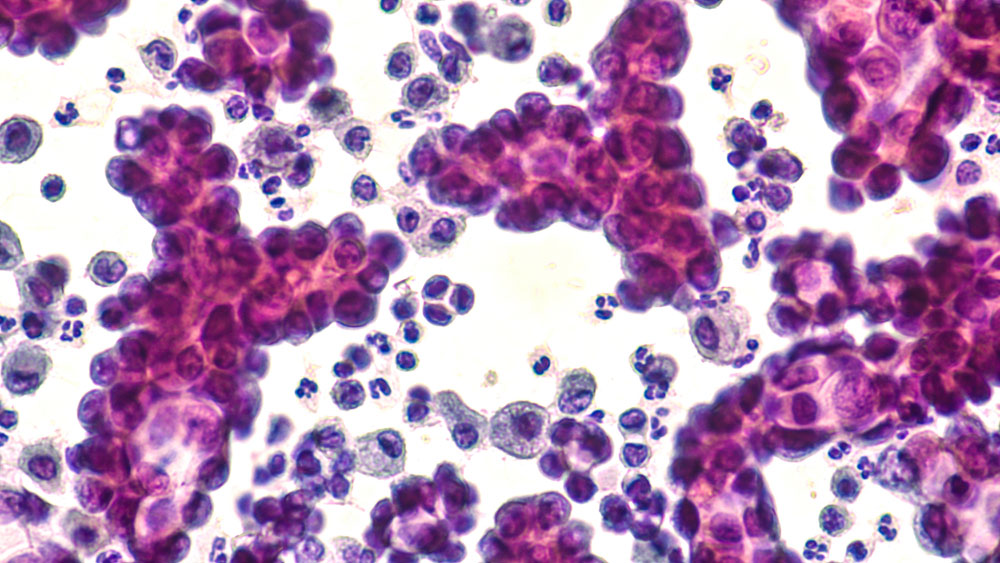
Biomarkers are characteristics of the body that you can measure and refer to such as proteins, genes, and other molecules that affect how cancer cells grow, multiply, die, and respond to other substances in the body. There are several types of biomarkers including:
- Clinical – biomarkers that are used in clinical resources or practice and can be used in clinical application
- Antecedent – biomarkers that are used to evaluate the risk of an individual developing a certain illness
- Screening – biomarkers that screen for subclinical diseases
- Diagnostic – biomarkers that help diagnose a disease by confirming the presence
- Prognostic – biomarkers used to predict the future of progression and how likely recurrence is
- Imaging – biomarkers that can be detected from an image
- Molecular – biomarkers that are non-imaging but have biophysical properties
An Individualized Treatment
Just like every individual and cancer treatment is unique, so are biomarkers. Every patient has a unique pattern that helps in aiding doctors in choosing a tailored treatment for them. This uniqueness also means that biomarker testing might not be an option and often not helpful in scenarios including:
- The patient is unable to safely get a biopsy that is needed for testing.
- here is not enough tumor tissue for a proper biopsy sample.
- he test does not find any biomarkers that match available therapies.
- he test identifies matching therapies that are off label that insurance typically does not cost.
- The test identifies a matching therapy that is in a clinical trial and the patient is not approved to participate.
Biomarkers are often referred to by a 3 or 4-letter abbreviation and some consider it more important than just identifying the type of cancer a patient has. These abbreviations are the key to understanding exactly what type of cancer, subtype, or other mutation the patient has. Once identified, patients can move forward with personalized treatments meant for their specific needs instead of wasting precious time and energy on treatments that could prove to be ineffective.
As biomarker tests become more prominent, the list of biomarkers grows. Currently, there are more than 80 biomarkers with potential use in cancer treatment today. Some of the of the more significant include:
Abbreviation
Definition
Cancer Correlation
PTEN
PIK3CA
MGMT
O-6-methylguanine-DNA methyltransferase – a gene that encodes a DNA repair enzyme, loss of MGMT may play a role in cancer formation and can also interfere with treatments that work by disrupting tumor DNA also interfere with treatments that work by disrupting tumor DNA
HER2
EGFR secondary mutation (T790M)
BRAF
Starting The Conversation
If a doctor has not initiated the conversation about biomarker testing and you are interested in having it done, express interest to your doctor. If you are not sure how to start the conversation about biomarker testing, try starting with a few simple questions:
- Is biomarker testing right for me?
- What type of biomarker testing would I need to do?
- If I have already begun treatment, can I still get comprehensive biomarker testing?
- If I do get biomarker testing, how will these affect my treatment course?
- What happens after biomarker testing if there are no options for me?



