
Identifying and Caring for Alzheimer’s Disease and Dementia
Caring for a loved one with Alzheimer’s Disease or Dementia can be demanding. There are constant worries of deteriorating behavior, making the best choices for their well-being, and if the care they are receiving is adequate. There are ways to ease this difficult journey. First is by remembering that you are not alone. More than 11 million people in the United States alone are unpaid caregivers for loved ones with dementia or Alzheimer’s. Second is understanding the difference between the two and how to specifically cater to each.
Commonly, Alzheimer’s and dementia are two terms that are used interchangeably when in fact one is a specific disease, and the other is the overall term for memory loss.
Alzheimer’s Disease
Alzheimer’s Disease is an irreversible, progressive brain disease that destroys memories, thinking skills, language problems and motor skills. This is due to the brain cell connections and how the actual cells degenerate and die. Currently more than 6 million people have been diagnosed with Alzheimer’s Disease and this number is predicted to more than double to 14 million by 2060.
Very rarely is Alzheimer’s caused by any specific genetics and is believed to be caused by a blend of genetics, lifestyle choices, environmental factors and many other complex brain changes that affect the brain over time. Due to these factors causing damage to the brain, Alzheimer’s disease tends to show exceedingly early clinical symptoms. Someone with late-onset Alzheimer’s disease will see symptoms in their mid-60s while early-onset can start as early as a person’s 30s. Alzheimer’s Disease also requires a medical diagnosis and there are some key symptoms to look out for.
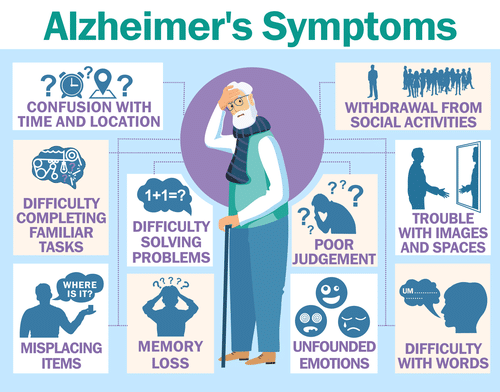
Other symptoms can include confusion in the evening hours, anger, depression, delusions, mood swings, restlessness, lack of restaurant, paranoia , wandering, inability to create new memories, personality changes, inability to combine muscle movements, loss of appetite, and meaningless repetition of words.
While monitoring symptoms, keep in mind there are seven stages of decline to recognize Alzheimer’s. These stages range from unnoticeable to extremely distinguishable. Recognizing these stages and where your loved one may be at is key to getting a care plan to not only help maintain quality of life but keep loved ones safe.
Normal Outward Behavior – you will not usually notice any change in your loved one since change happens unnoticed in the brain in the beginning.
Very Mild Changes – this stage can simply include mishaps such as forgetting words or misplacing objects.
Mild Decline – this stage introduces a noticeable change in a loved one’s thought and reasoning processes.
Moderate Decline – this is when the changes you noticed in stage three become more prominent. People start to forget details, small personal details, and difficulty with tasks.
Moderately Severe Decline – loved ones could have trouble remembering their address, dates, and how to dress appropriately. This is typically when supervision might need to be started.
Severe Decline – when a person can recognize faces but not names. This stage is when delusions can set in and there will be a decline in motor functions. You also might notice a change in their sleeping pattern or weight loss.
Very Severe Decline – this stage is when basic abilities such as eating, and walking begin to decline. This final stage is when caregivers are absolutely needed to ensure quality of life.
Dementia
Unlike Alzheimer’s, dementia is not a disease. It is also not a normal part of aging. It is the overall term for the loss of memory, language, problem-solving abilities, and social abilities. Alzheimer’s disease is the most common type of dementia, affecting 44 million worldwide.
Dementia is caused by abnormal brain changes that are caused by damaged nerve cells and their connections in certain areas of the brain. There are several types of dementia that can affect people differently and that have various symptoms. The common denominator between types of dementia is protein deposited in part of the brain.
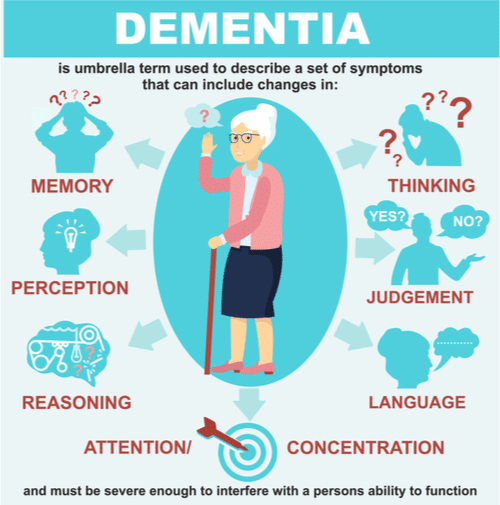
The image above depicts the overall signs of generalized dementia. Since dementia is just an overall term though there are several irreversible, progressive dementia types besides Alzheimer’s disease. Four common types, plus their common symptoms, are:
Vascular Dementia is caused by damage to the vessels that supply blood to your brain. This can cause strokes or cause other serious brain affects. Common symptoms are difficulty with problem solving, loss of focus, restlessness, depression and slowed thinking.
Frontotemporal Dementia is caused by breakdown of the nerve cells and the connections they have to the frontal and temporal lobes of the brain. This type is typically characterized by increasingly inappropriate social behavior, loss of empathy, loss of inhibition, loss of judgment compulsively wanting to put items in their mouth and eating inedible objects.
Mixed Dementia is a condition where a person has a combination of more than one type of dementia. The most common is Alzheimer’s and vascular dementia. Typically, there will be a more prominent type of dementia and symptoms will match that, but symptoms vary person to person.
Lewy Body Dementia is a progressive dementia that causes a decline in thinking, reasoning, and independent functions. This is because of abnormal microscopic deposits that damage brain cells. Symptoms include confusion and alertness that drastically varies, well-formed hallucinations and sleep disturbances.
Caring For Alzheimer’s Disease or Related Dementia
“There is a moral task of caregiving, and that involves just being there, being with that person and being committed. When there is nothing that can be done, we must be able to say, “Look, I’m with you in this experience. Right through to the end of it.” – Dr. Arthur Kleinman
If a nursing home is not currently an option, the bulk of responsibility falls on the family member turned caregiver’s shoulders. Though adjusting your life around a loved one with Alzheimer’s or dementia can be challenging, there are a few ways to help ease the transition.
Creating a safe environment is a great place to start. Alzheimer’s and types of dementia both impair judgement, vision, problem-solving abilities and increase risk of injury. You can create a safe-space by taking fire precautions, using locks on cabinets with anything potentially dangerous and avoid tripping hazards in frequently walked areas.
Overcoming Communication Boundaries
It may seem frustrating trying to communicate with someone who is slowly losing their ability to, but it is not impossible. When communicating be sure to set a positive mood for the interaction from the start. People with Alzheimer’s are already frustrated enough trying to convey what they say, if you start a conversation frustrated, they will likely follow suit. You can also keep their attention by limiting distractions, maintaining eye contact, using their name, and introducing yourself and who are in relation to them.
Now that they are actively listening to you, talk slowly and clearly. If you need to ask questions, keep them simple and refrain from giving open ended questions or too many choices. If you need to complete a task, break it down into steps and go through them one at a time. Alzheimer’s disease and dementia cause people to feel confused, easily distracted, unsure of their choices or themselves. Reinforce conversations and the completion of tasks with affection and reassurance.

When you need to handle the times where the conversations are not going so smoothly, you can always distract and redirect. Anger and agitation are a prominent symptom of dementia, if your loved one is upset, you can easily change the subject, environment or bring in someone else to the conversation as a change of pace.
Sometimes you might face a complete communication breakdown, where you just cannot seem to connect at all. This would be a time to bring up the comfort of old memories or something that they are passionate about. Topics that are familiar, and do not rely on short-term memory, will always be the easiest to talk about because they are usually still the most distinguished in the mind.
Managing Day-To-Day Tasks
Just as Alzheimer’s progresses, so will tasks due to the loss of overall interest and motor functions. While able, have your loved one participate in as many tasks as they can. This can include dressing themselves, cleaning themselves, helping prepare a meal, cleaning up, or folding laundry – basically anything that pushes the idea of independence with supervision.
One of the hardest things for a person with dementia to lose is their independence. Many will hold on to as much independence for as long as mentally and physically possible. In addition to letting them do tasks stated above such as dressing and cleaning themselves, you should also give them options. Involve your loved one in choices such as picking out their outfit, what they want to eat, or what activities they want to do.
Having a daily schedule that includes your loved one’s preferences will help reduce frustrations. Even though Alzheimer’s and dementia cause memory loss, loved ones can still become used to and follow a routine when repeated. Everyday should not be expected to be the same so plan for occurrences such as spontaneous activities or extra difficult days.

Alternative Options
It is not always possible for a person to care for a loved one, at home, and unpaid. As Alzheimer’s or dementia worsens, day-to-day care also increases. There are two options for families who need help maintaining their loved ones’ quality of life.
The first is home care which is when a professional caregiver can come to the patient’s home to prefer care. Their care includes dressing, feeding, monitoring symptoms, maintaining diet, household chores, money management, physical therapy, and all other care needs. Home care is beneficial because it keeps patients in a comfortable environment.
Second is a nursing home. Nursing homes are a great option when patients or families do not have a safe, stable environment to ensure the patient’s well-being. Other factors could be work obligations or needing more skilled care. Nursing homes designed for Alzheimer’s and dementia patients are created to have warm, inviting environments and extra precautions in place to help stop wandering and ensure a safe, home-like environment.
Care That Fits Your Family
Regardless of if you chose to care for a loved one yourself, utilize home care or decide on a nursing home – the individual care and safety of a person with Alzheimer’s or dementia remains a top priority. How your family chooses to care for a loved one enduring memory loss is a personalized experience based on specific needs. While patients experience loss of memory, independence, motor skills, social skills, and problem solving abilities – they rely on some type of caregiver to maintain daily living. It is not an easy job to care for someone with Alzheimer’s or dementia, but it is a truly selfless act to do so.



